Did you know atopic dermatitis hits 10 to 20 percent of kids and 5 to 10 percent of adults across the globe? It’s more than just dry, itchy skin. It’s a battle with red, inflamed areas that affect how we live. Knowing how genes, our immune system, and environmental factors mix can help us tackle it.
This skin issue can start in the young years and might stick around into adulthood. It’s not just about the skin. It often brings along food allergies, hay fever, and asthma. This is called the “atopic march.” A gene called FLG affects our skin’s defense. Both the world around us and our own health history influence its impact.
In this article, you’ll get the scoop on the wide-ranging reasons behind atopic dermatitis. We’re diving into the world of genetics and environmental factors. A lot of people deal with this, and understanding it is key.
Key Takeaways
- Atopic dermatitis affects 10-20% of children and 5-10% of adults.
- Genetic factors play a significant role, particularly the FLG gene.
- Environmental triggers include allergens like dust mites and pet dander.
- It is often associated with other allergic conditions, including asthma and food allergies.
- Understanding triggers can help in managing the symptoms effectively.
An Overview of Atopic Dermatitis
Atopic dermatitis, or eczema, is a common chronic skin problem. It often starts in early childhood, between 2 months and 5 years old. By five years old, many kids show signs of eczema. Yet, it can also start in puberty or even in adulthood.
The main symptoms of eczema are dry, itchy skin, and red patches. These patches might weep or get crusty. Babies often get eczema on their cheeks and scalp. Adults, however, usually have it on their wrists and ankles. This condition can make everyday life hard, causing discomfort and disrupting sleep.
In industrialized countries, atopic dermatitis cases have increased 2-3 times. It affects about 10.7% of kids and 7.2% of adults in the US. Around 60% show symptoms in their first year. By age five, 90% have experienced eczema. Sadly, 20% of kids who get eczema before age two will have long-term symptoms.
There’s no cure for atopic dermatitis, but it can be managed. The aim of treatment is to ease symptoms and better the skin’s health. Dermatologists work on finding safer treatments. Everyday use of moisturizers is key. They soothe the skin and prevent outbreaks, showing why early and continuous treatment is vital.
Check out this detailed atopic dermatitis overview for more information on the condition and how to treat it.
Understanding the Main Causes of Atopic Dermatitis
Atopic dermatitis, or eczema, is very common. It affects over 9.6 million kids and 16.5 million adults in the U.S. The main causes include genetics and the environment.
Genes play a big role. For example, changes in the FLG gene can make the skin barrier weak. This makes the skin more open to irritation and allergens. If eczema, asthma, or allergies run in the family, the risk goes up.
Then there are environmental triggers. Things like dust mites, pet fur, and dirty air can make it worse. Stress can also trigger flare-ups. It’s important to avoid these triggers as much as possible.
So, atopic dermatitis is complex, involving both genes and the environment. Knowing about these factors can help manage this skin issue better.
Genetic Factors Contributing to Atopic Dermatitis
Genetic factors are key in the onset of atopic dermatitis (AD). Changes in genes, especially the FLG gene, hurt the skin’s barrier function. By studying these genetic changes, we understand why some people are more prone to AD.
Role of the FLG Gene in Skin Barrier Function
The FLG gene helps make profilaggrin. This protein is vital for a strong skin barrier. When the FLG gene changes, the risk of AD goes up. Research shows that half of the kids with serious eczema have these changes.
Kids with these gene changes often get AD earlier. If symptoms start before five years old, the risk is even higher. FLG changes are also more common in those with AD than in healthy people.
Other Genetic Variations Associated with Atopic Dermatitis
AD isn’t just about the FLG gene. Other gene changes are also linked to it. These include CLDN1, Tmem79/matt, and some EDC genes. They may weaken the skin barrier or make someone more likely to get AD.
For example, CLDN1 changes can weaken skin’s tight junctions. Tmem79 missense changes increase AD risk too. Researchers have found rare variants that show the genetic complexity of AD. Knowing about these varied genetic factors helps us understand AD’s risks better.
| Genetic Factor | Impact on Atopic Dermatitis |
|---|---|
| FLG gene | Major risk factor; mutations lead to impaired skin barrier function. |
| CLDN1 gene | Mutations may compromise tight junctions, increasing susceptibility. |
| Tmem79/matt gene | Missense mutations can predispose individuals to atopic dermatitis. |
| LELP1 gene | Associated with IgE levels and early onset of atopic dermatitis. |
Immune System Dysregulation in Atopic Dermatitis
Atopic dermatitis (AD) is mainly about the immune system not working right. This causes immune responses to act out of order. Because of this, people with AD have skin that gets inflamed, turning red and itchy. High levels of immunoglobulin E (IgE) and certain cytokines are found in those with AD. These contribute a lot to their inflammation.
How Immune Response Triggers Skin Inflammation
The connection between immune system issues and skin inflammation in AD is key to understanding the disease. People prone to allergies usually have overactive immune responses. This can be due to genetic or environmental factors.
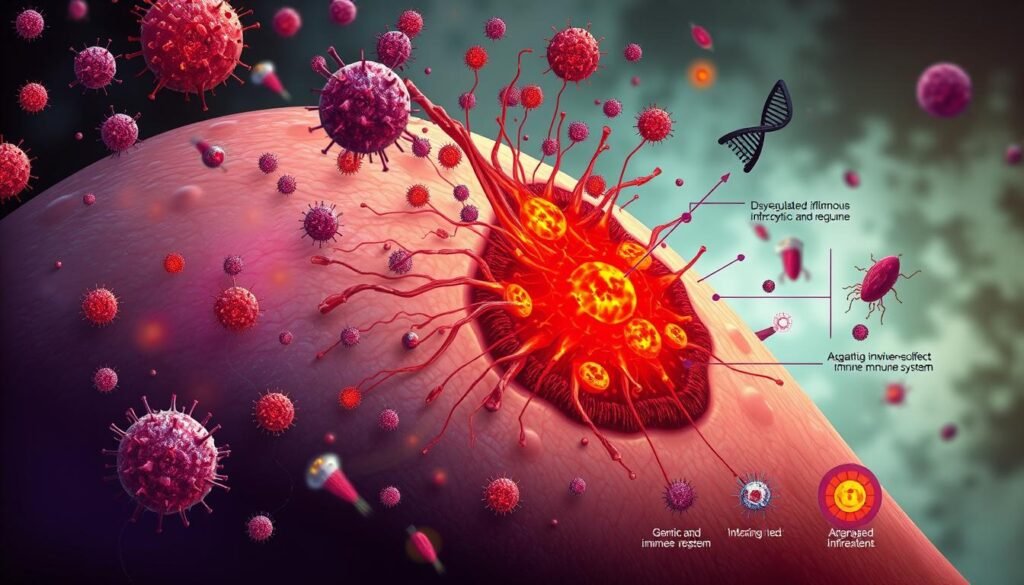
Genes, especially the FLG gene, play a big role in weakening the skin’s barrier. This makes inflammation easier. Studies show that mutations in this gene make people more likely to get infections and have skin issues. Around 80% of infants with AD tend to produce IgE. This is linked to allergic conditions.
Knowing how the immune system messes up is crucial for creating better treatments. Treatments like anti-IL-4 and anti-IL-13 have been effective. They target specific cytokines involved in the inflammation cycle in AD.
Various immune cells and cytokines keep the inflammation going in AD. The increase of type 2 cytokines, like IL-31, in skin lesions shows how the immune response causes discomfort. For more about how immune dysregulation impacts AD, check out this link.
| Immune Components | Role in Atopic Dermatitis |
|---|---|
| Immunoglobulin E (IgE) | Triggers allergic reactions and inflammation. |
| Type 2 Cytokines (IL-4, IL-13) | Maintains chronic inflammation. |
| Filaggrin (FLG) | Critical for skin barrier integrity; mutations increase infection risk. |
| Memory T cells | Involved in persistent skin inflammation and response to injury. |
Environmental Risk Factors for Atopic Dermatitis
Knowing about environmental factors is key for those with atopic dermatitis. These factors greatly affect how severe and often their condition becomes. Allergens, irritants, climate, and pollution play a big part in making symptoms worse.
Impact of Allergens and Irritants
Common allergens such as dust mites, pollen, and pet dander often lead to worse symptoms. Everyday products with irritants like soaps and detergents add to the problem. These environmental triggers can make skin more inflamed and irritated. For tips on dealing with these issues, check out this helpful site.
The Role of Climate and Pollution
Changes in weather, especially dry or cold air, can reduce skin moisture. This makes atopic dermatitis symptoms more intense. Pollution is also harmful. It can cause inflammation and hurt the skin’s protection. People in polluted cities face higher risks for their skin conditions. By understanding these environmental triggers, they can better avoid them and manage symptoms.
Causes Atopic Dermatitis: The Interplay of Genetics and Environment
Atopic dermatitis comes from genetics and the environment. Science shows that those with family history are more at risk. About 70% of people with this skin condition have relatives also affected by it. This points to how important heredity is.
Environment plays a big role too. Things like allergens and pollution make the condition worse. Living in the city, with more pollution, often leads to more cases than in the countryside. Indoor and outdoor pollution damage the skin’s barrier, making symptoms worse. Stress in pregnant mothers can also increase a child’s risk.
Climate affects skin health as well. Dry weather can raise the chances of getting atopic dermatitis. Likewise, using soaps and cleaners often can harm the skin more.
To really understand atopic dermatitis, we must look at genetics and environment together. Researching these connections helps create better treatments.
If you want to learn more about eczema, check out this info. To explore related conditions like hand eczema, and find out how to manage them, click here.
The Atopic March: Progression of Allergic Disorders
The atopic march is about how allergic problems start and grow, often starting with eczema when kids are young. Atopic dermatitis is the first sign and can lead to other issues. Many kids with it may later get food allergies, allergic rhinitis, and asthma. How common it is in kids varies, with rates from 0.3% to 20.5% in different places.
In the US, about 17.2% of kids aged 5 to 9 have atopic dermatitis. Almost half of these kids show signs in the first six months. By the time they’re five, 85% of them have felt its effects. Sadly, fewer than half will be totally free of eczema by age seven. And only 60% will outgrow it by adulthood.
As atopic dermatitis sticks around, the chance of getting worse allergic problems gets higher. About 70% of those with bad atopic dermatitis will get asthma. This is much more than the 20-30% with milder versions. This shows how childhood eczema and later asthma are linked. It’s crucial to spot and treat these issues early to stop more problems.
There’s a clear link between allergic rhinitis and asthma, with 75% of asthma patients also having rhinitis. Sometimes, 80% of people with rhinitis also have asthma. These numbers show why it’s key to watch and tackle eczema early. This can help avoid more allergies.
Knowing about the atopic march shows how connected these conditions are. Looking at everyone’s different health, surroundings, and how they live gives clues on preventing and managing these issues. For more on how these allergic conditions link, look at this study on the atopic march.
Psychological Factors: Stress and Atopic Dermatitis
Stress plays a key role in atopic dermatitis. This condition affects about 20% of kids and 7-10% of adults in the USA and Europe. Stress is known to make the symptoms worse and increase flare-ups. Knowing how stress affects skin health is crucial for those dealing with this condition.
How Stress Affects Skin Health
Studies show chronic stress makes atopic dermatitis worse for many people. Stress leads to higher itch levels, often more intense than other triggers. This makes managing atopic dermatitis hard, especially when stress is the cause.
Things that add to stress include:
- Family problems
- Financial difficulties
- Work overload
- School exam pressures
- Lack of structure at work
- Unforeseen personal events
Stress affects skin through complex body reactions. The stress triggers the hypothalamic-pituitary-adrenal (HPA) axis. This causes hormone changes. It increases certain hormones that can affect the skin’s immune responses.
Stress also makes nerve fibers in the skin release substances that inflame it more. This inflammation adds to the discomfort of atopic dermatitis. Understanding this shows why stress management is important in treatment plans.
Identifying and Managing Triggers
Effective management of atopic dermatitis requires knowing what triggers flare-ups and finding ways to reduce their effect. These triggers can come from different areas such as the environment, genetic factors, and everyday habits. It’s crucial to identify these triggers for better management of atopic dermatitis and healthier skin.
Common Triggers in Daily Life
In daily life, many things can trigger atopic dermatitis flare-ups. Knowing what these triggers are can help prevent them. Below are common triggers seen daily:
- Environmental factors such as dust mites and pet dander.
- Specific fabrics that can irritate sensitive skin, including wool and synthetic materials.
- Skin irritants such as harsh soaps or detergents.
- Extreme weather conditions, including cold and damp environments.
- Allergens and irritants found in the home or workplace, including perfumes and cleaning products.
- Stress, which can worsen skin conditions and overall health.
- Food allergies that cause irritation, especially in kids.
To manage atopic dermatitis well, it’s key to have a care routine that suits your specific triggers. This includes keeping your skin moist, choosing the right clothing, and avoiding known allergens. Managing stress well can also lower flare-up severity.
Discovering better ways to spot triggers can greatly improve daily life with atopic dermatitis.
| Trigger Type | Description | Management Strategies |
|---|---|---|
| Environmental | Dust mites, pet dander | Regular cleaning, use of air purifiers |
| Fabrics | Wool, synthetics | Opt for soft, breathable materials |
| Irritants | Harsh soaps, chemicals | Choose gentle, fragrance-free products |
| Weather | Cold, damp conditions | Dress in layers, use humidifiers |
| Stress | Emotional triggers | Practice relaxation techniques |
| Food | Common allergens | Keep a food diary, consult with an allergist |
Conclusion
Atopic dermatitis is a complex skin condition with many causes. It involves genetics, the immune system, and the environment. Knowing why it happens is key for managing it well.
In the U.S., it affects up to 12.7% of kids and 7.6% of adults. This shows how important it is to be aware and take action.
New research has found how gene changes, like filaggrin mutations, play a role. These discoveries link our genes to our skin’s health. Also, things around us, like allergens and pollution, make atopic dermatitis worse. This shows how outside factors play a part.
More studies are helping us understand this condition better. They’re showing us how it develops and how we can treat it better in the future.
Dealing with atopic dermatitis requires a detailed strategy. It means knowing your risks, what makes it worse, and how it affects your mood. By doing this, people can see big improvements in their life despite the condition.